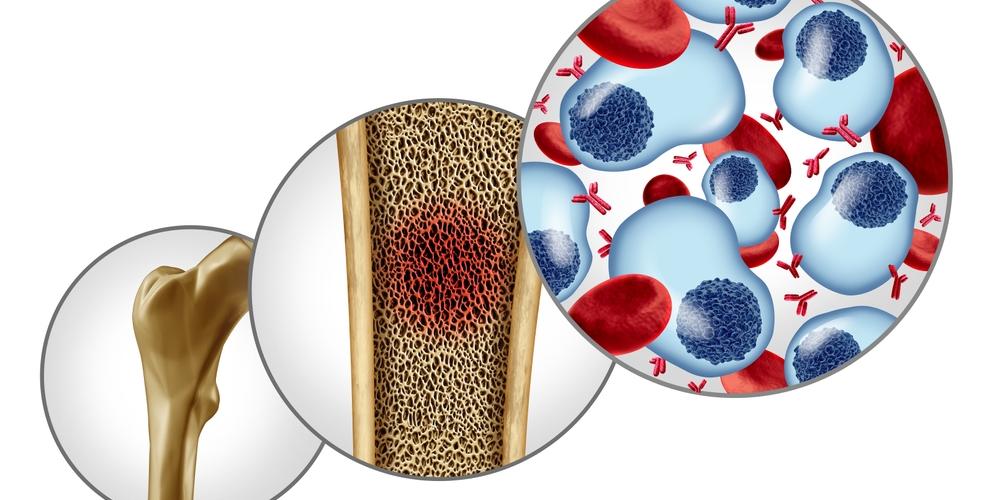
Dr. Heleen Hanssens from the Molecular Imaging and Therapy (MITH) Research Group at Vrije Universiteit Brussel (VUB) has conducted research on the application of CAR T-cell therapy in multiple myeloma, a form of bone marrow cancer that remains considered incurable.
Dr. Hanssens explains: “CAR T-cell therapy is an innovative treatment that harnesses the patient’s own immune system to attack cancer. T-cells, a type of white blood cell, are extracted from the patient’s blood and genetically modified. These modified T-cells are equipped with a ‘chimeric antigen receptor’ (CAR), a kind of radar that allows them to recognize and target cancer cells. The CAR T-cells are then reintroduced into the patient’s body to combat the tumor. While many new therapies for multiple myeloma have been developed in recent years, the disease often returns eventually. My research focuses on optimizing CAR T-cell therapy to increase its long-term effectiveness.”
Dr. Hanssens’ work aims to break the recurring pattern of relapse by utilizing special antibody fragments known as VHH or 'nanobodies', derived from a specific type of antibody found in camelids. These nanobodies are smaller and more stable than conventional antibodies, which helps extend the lifespan of CAR T-cells. By using advanced imaging techniques and molecular analysis, she gained new insights into the role of these antibody fragments in enhancing CAR T-cell effectiveness.
New Markers and Advanced Screening
One of the challenges with current therapies is that over time, cancer cells can lose certain molecular markers, making it harder for CAR T-cells to recognize and destroy them. Dr. Hanssens identified two key markers for multiple myeloma cells, including a universal marker found in nearly all myeloma cells, even after multiple treatments. She also worked on identifying patient-specific markers, which could help target isolated residual cancer cells in the later stages of the disease.
"The nanobody screening platform is versatile and not limited to multiple myeloma."
“A second focus of my research is improving the CAR T receptor design itself. Traditional antibody fragments are used to recognize cancer cells, but these fragments are often unstable, leading to random activation and exhaustion of CAR T-cells. This issue is less common when using nanobodies. We found that the specific nanobody used has a significant impact on the therapeutic potential of the CAR T-cell. At the same time, we realized that the classical method of nanobody selection is not suitable for developing effective CAR T-cells,” Dr. Hanssens explains.
To address this, Dr. Hanssens' team developed a new screening platform for nanobodies, directly tailored for use in CAR T-cells. This allows for quicker and more accurate identification of the most effective nanobodies against specific cancer cells, thereby optimizing multiple myeloma-specific CAR T-cells. The nanobody screening platform is versatile and not limited to multiple myeloma. It’s a universal process that can be used to identify nanobodies for various cancer markers, potentially expanding the application of CAR T-cell therapy to other cancer types.
According to Prof. Nick Devoogdt, Dr. Hanssens’ supervisor and head of the MITH research group, this research represents a critical step in advancing cancer therapies: “Our findings enable us to design optimized CAR T-cells for various types of cancer in a universal way, helping us develop more durable treatments.”